Running with an Elevated Heart Rate After COVID
As a journalist and an athlete, I like answers. And with COVID-19, there aren’t a lot of clear ones. I found this to be true after I got COVID-19 in March of 2022. I experienced lung and heart problems after COVID, including an elevated heart rate.

It was hard to find information as to why my heart rate was spiking, if it was a cause for concern, and IF I should not run until it was regulated. I found that from athletes I personally know and fellow runners in my Instagram community, having an elevated heart rate after COVID was fairly common.
Table of contents
- My Experience with Cardiac Symptoms After COVID
- FAQs about having an Elevated Heart Rate after COVID
- What the Research Finds About Cardiac Symptoms After COVID
- Why does my heart beat faster after having COVID?
- Is it normal to have a high heart rate after COVID-19?
- All of my tests came back normal, but I am still having chest pain and a rapid heart rate, what is going on?
- When should I be concerned about my elevated heart rate or heart palpitations?
- Could I have heart damage from COVID-19?
- What is the autonomic nervous system and how does COVID-19 affect it?
- How do you treat autonomic system dysfunction?
- What is Long COVID?
- Who is more at risk for long COVID and cardiac symptoms after having COVID?
- Can I start running if I am still having cardiac systems after having COVID?
But did that mean it was safe to run with a higher heart rate? I still had so many questions. So, I’ve dug into the research to share what I have learned about cardiac symptoms after COVID and long COVID to help guide you in your training and treatment.
Note: I am NOT a doctor, though this information comes from doctors and researchers. Always follow your doctor’s guidance.
My Experience with Cardiac Symptoms After COVID
I want to begin with a quick overview of what happened to me with my COVID recovery. Obviously, every case with COVID is different, which is a huge reason why it is all so confusing. But maybe, my experience can help you find answers or recover quicker.
In April of 2021, I got my second COVID shot and experienced severe chest pain later that day. I ended up in the ER with pleurisy (inflammation of the lung lining). It took me 6 weeks to recover, including a 6-week break from running. Nothing like this has ever happened to me before.
In late March of 2022, I went for a 16-mile run and felt pretty bad. I continued to feel bad the next morning. My stats on all my wearable fitness tracker, WHOOP, were all off including my Heart Rate Variability which is an indicator that you may be getting sick.
I tried to do a shake-out run and my heart rate was very high. I returned home and took a COVID-19 test which tested positive.
My Progression of COVID-19 Symptoms
I felt very sick for about 3 days including a deep cough, fatigue, and shortness of breath. A week later, I felt better and attempted to run. After four days of light running, I regressed.
I experienced heart problems after COVID including heart palpitations, heart rate spikes, chest pain, shortness of breath, and what felt like an irregular heartbeat.
I went to a walk-in clinic and got my blood drawn, a chest X-ray, and an EKG which all came back normal.
A week later, I continued to feel ill. My WHOOP kept showing my vitals out of whack including heart rate spikes. For example, when I was putting peanut butter on a bagel, my heart rate was in the 140s.
My post-COVID-19 Diagnosis & Treatment

I went to see a doctor. She diagnosed me with chest wall inflammation and sympathetic overdrive. She prescribed steroids, an inhaler, and rest.
I took a few days of complete rest and then began walking. About 10 days later, I did a 3-mile jog, alternated run days, repeated mileage, and progressed. (Read more on my return to run plan below).
My heart rate was unusually high on my runs. My resting heart rate dropped to 41 and then went up to 57 (46 is my norm). And I had brain fog and fatigue no matter how much I slept. In the third week, I felt markedly more energetic with less brain fog.
About 5 weeks into my recovery, everything began normalizing minus some chest pain and an elevated heart rate.
Why I Wrote This Article
The time scales for recovery differ for everyone. Still, I believe my COVID-19 recovery journey and research may be helpful to you.
I think while the new variants of COVID-19 may produce a milder infection, it’s important for people (especially runners) to understand it is still more taxing on the body than a bad cold and it’s important to be conservative in your return to running.
As Dr. William Li, physician, scientist, president and medical director of the Angiogenesis Foundation, and author of Eat To Beat Disease: The New Science of How Your Body Can Heal Itself, told me:
“While COVID infection has become much milder for most people, the unpredictable nature of serious aftereffects is still something the medical community is very concerned about.”
FAQs about having an Elevated Heart Rate after COVID
What the Research Finds About Cardiac Symptoms After COVID
A study, published in Nature, of more than 37,000 people recovering from COVID-19, found I was not alone in my lingering symptoms.
Tracking the data from wearables like FitBit, the researchers revealed that:
- After 9 days of first reporting symptoms, the participants’ resting heart rate dropped.
- Then, the heart rates rose and remained elevated for months. The resting heart rate was elevated 5 beats, on average.
- On average, participants had elevated heart rates for 79 days.
- Sleep and physical activity returned to baseline more slowly.
Why does my heart beat faster after having COVID?
Researchers and doctors believe the prolonged heart rate elevation is a sign that Covid-19 disrupts the autonomic nervous system,
which regulates basic physiological processes.
This explains why the heart races, palpitates and causes dizziness. This may also explain fatigue and brain fog.
“Lots of people who get Covid end up getting autonomic dysfunction and a kind of ongoing inflammation, and this may adversely affect their body’s ability to regulate their pulse,” explained one of the researchers, Dr. Jennifer Radin.
Is it normal to have a high heart rate after COVID-19?
Yes. Research shows it is normal to have a higher heart rate for more than two months after recovering from COVID-19.
In my personal experience and an unofficial Instagram poll of more than 100 runners, 85 percent had elevated heart rates. Most of these heart rates normalized in time
(Not sure when to rest, check out my article: When to Skip a Workout & How to Adjust Your Schedule)
All of my tests came back normal, but I am still having chest pain and a rapid heart rate, what is going on?
You’re in good company. Many others and I have had tests like blood tests, an EKG, x-rays, and cardiac MRIs return to normal yet still experience an elevated heart rate, shortness of breath, and chest pain.
Doctors, including my own and those at UAB, attribute this to sympathetic overdrive along with chest wall inflammation which your body should heal in time.
However, if you are concerned about your condition, consider seeing a cardiologist to get more tests and wear a Holter monitor, which monitors your heart around the clock.
“This can document when your heart rate changes, even if you cannot feel it,” explains Dr. Li.
One possible explanation for someone who develops an abnormal rise in heart rate when standing could be a condition called Postural Orthostatic Tachycardia Syndrome (POTS).
POTS is caused by an abnormality in the autonomic nervous system, which regulates blood flow back to the heart. You likely do not have POTS if your heart rate decreases each time you run or walk.
When should I be concerned about my elevated heart rate or heart palpitations?
You should be concerned about your rise in heart rate or heart palpitations, which feel like your heart is pounding, fluttering, or beating irregularly, if:
- Your heart rate does not gradually go down after exercise.
- You have chest pain.
- The occurrences are becoming more severe or more frequent, and/or
- You have a known heart condition, injury, or weak heart muscle.
- If you feel lightheaded, dizzy, or collapse during an episode of tachycardia, or elevated heart rate.
“In this case, the body is unable to compensate so the brain may not be getting enough oxygen from blood flow. This is an automatic red flag, and a signal to seek help,” warns Dr. Li, who has appeared on GMA and CNN and in The Atlantic and Time Magazine.
This is not an exhaustive list, and I am not a doctor. If you are concerned, you should go see one.
Could I have heart damage from COVID-19?
There have been fears that COVID-19 could cause myocarditis (inflammation of the heart muscle) and pericarditis (inflammation of the sack around the heart), leading to direct damage of the heart muscle.
However, this is rare.
Admittedly, when my heart rate was at the height of its irregularity accompanied by chest pain, I searched Dr. Google and was close to self-diagnosing with myocarditis as the symptoms were very similar (minus intense swelling).
However, the cause of the change in heart rate or irregular heartbeat is likely a hormonal imbalance triggered by the virus that impacts the function of the autonomic nervous system.
What is the autonomic nervous system and how does COVID-19 affect it?
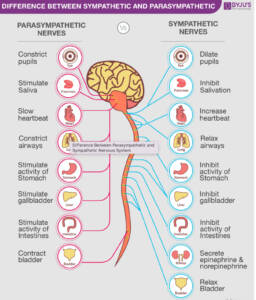
The autonomic nervous system controls unconscious bodily functions such as blood pressure, heart rate, breathing rate, digestion, body temperature, and metabolism.
It is usually divided into two parts: the parasympathetic nervous system and the sympathetic nervous system.
- The parasympathetic system is often called the “rest and digest system” and controls functions that happen at rest.
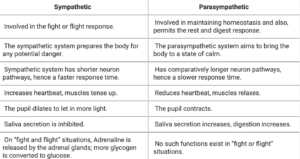
If your body perceives a threat like the COVID-19 virus, the sympathetic nervous system may overact, causing your heart to rate and breath rate to quicken.
This is what is thought to have happened to me in what my doctor called a sympathetic nervous system overdrive.
How do you treat autonomic system dysfunction?
The treatment for an imbalance of the autonomic systems varies depending on the symptoms and severity.
The treatment or way to quiet the sympathetic nervous system is often to do calming activities such as:
- gentle walks
- rest
- sleep
- deep breathing
- yoga, and
Doing something that stresses the body and elevates the heart rate such as running could worsen or elongate the COVID recovery process.
What is Long COVID?
The lingering after-effects of a COVID infection are called Long COVID and are not related to damage by the virus itself but by the body’s immune response to COVID-19.
The most common symptoms of long COVID include:
- chest pain
- heart palpitations
- abnormally high heart rates
- heart palpitations
- shortness of breath,
- and difficulty doing their normal exercise routines
Doctors theorize that long COVID and related symptoms are caused by a dysfunction of the autonomic nervous system (caused by a hormonal imbalance) thereby disrupting functions such as blood pressure, heart and breathing rates, body temperature, digestion, and metabolism.
Long COVID or long-haulers can last weeks or months and can be severe and life-altering, sadly.
Who is more at risk for long COVID and cardiac symptoms after having COVID?
Doctors say long COVID can affect anyone, even if your case is mild. It can also begin after you thought you had recovered.
There is also no evidence if anything such as exerting oneself too soon by running can contribute to long COVID.
Can I start running if I am still having cardiac systems after having COVID?
You can return to run if you still have cardiac systems after having COVID such as an elevated heart rate as long as your doctor clears you!
“If there is any lightheadedness, dizziness, or feeling of passing out — or any chest pain, shortness of breath, or palpitations, it’s time to seek out a doctor to at least make sure there is nothing serious that must be addressed. When it comes to your heart, it’s best to take no chances,” says Dr. Li.
If you do not have heart damage or a heart condition, in most cases cardiovascular exercise (for 30 minutes a day, 5 days a week) is beneficial for your COVID recovery. Get guidance from your doctor.
The key for your return to running after COVID is taking a gradual approach. For example, when you are feeling more like your normal self:
- Walk every other day for 4 days for 30 minutes. When that feels good, add a consecutive day. Then another.
- After being able to walk for 5 days for 30-60 minutes with no issue, try an easy run of 1-2 miles.
- If that feels good, begin running every other day. You can walk in between.
- After doing a run two times of a specific distance, you can add 5 minutes or a mile to your run (depending on your fitness level and how you feel).
- Continue to repeat mileage one time and alternate days.
- When you can run for an hour with no issue, try a consecutive day run.
- Be sure to keep your pace very easy—much easier than your usual easy pace.
- Continue to have at least one total rest day.
- When your mileage gets higher (like over 4 miles, don’t repeat mileage. Alternate between higher and lower mileage).
Read more about how to return to run here.
How I Returned to Running with Cardiac Symptoms After COVID:
I began a gradual return to running even though my heart rate was elevated more quickly and my resting heart rate was higher than normal. I also still had some minor chest discomfort on the right side of my chest which was diagnosed as muscular inflammation.
- I walked for about 10 days and began with a 3-mile jog. I tried another 3-mile jog two days later.
- When that felt okay, I progressed to 4 miles and so on.
- When I got to 6 miles comfortably, I tried running for consecutive days.
- Then, I progressed my mileage as normal, taking it day by day.
- I learned that keeping my easy pace about 1 minute per mile easier than my norm was key to recovering well and preventing chest pain.
What’s been your experience with COVID?







Whitney, Thank you so much for writing this, everything you experience happened to me as well it was a good 3-6 month battle of up and down symptoms. I am on my way and determined to get back to my pre Covid self.
I am SO happy to hear you are on the path to normalcy!!
This was a great summary and consistent with what my circle of athlete-friends have said about their symptoms. Hoping to avoid the current (minor) surge as race season is approaching…
Thanks for reading! & me too! Seems like everyone is getting it right now 😱
Thanks a lot for posting this. I have read many articles on the internet but found this to be most complete. This really eases me a lot! It’s 2:30am and I’m wide awake because my wife is experiencing most of the above symptoms. The doctors to whom we’ve shown remain clueless and surprisingly they don’t even know half of what you have covered in the post above.
Best Regards
Shivam
It is scary, Shivam! I hope your wife recovers quickly. I found knowing what is going on helps ease the mind & calm the nervous system!
Thanks for this post! I’m avery healthy, avid 44 y/o exerciser that alternated between jogging, cycling and weight lifting. I got CoVid recently despite vax and booster. I did not get paxlovid. Initially it felt like a flu but then unfortunately I ended up with after-effects including facial numbness, heart fluttering, shortness of breath and elevated heart rate. Steroids got rid of the numbness and an inhaler has helped a lot with the shortness of breath. It’s been 4 weeks and just now is when I’m starting to feel a bit more normal although I still get tired easily and my heart rate is still at least 20-30 points over normal when exercising. Your post was exactly what I am dealing with, so thanks so much for the information! It helped my drs figure out what to do next. My question now is- will this happen to me again if I get covid again? How can I avoid these symptoms if I do get it again? I’m hoping my pcp can give me some advice on that.
I am glad you are feeling better! From people I know & what I have heard, it’s less likely for it to happen again if you get COVID again within 6 months or so of your first contraction. But I definitely check with your doctor!
Thanks so much for writing this. I started my return to sport based on the guidance of my doctor who referred me to a recent journal article written by the Chief Medical Officer at the AIS. I progressed through to the stages where I should return to normal activity, but then I had a huge amount of stress from work and now my HR is elevated in a zone 2 ride and my garmin body battery doesn’t recover like it normally would.
I was pretty worried about it, but it makes sense given the impact of covid on the autonomic nervous system.
I should have known better than to return to work!
Guess it’s going to be a slow recovery, but it is unlikely to be anything too serious.
I am so sorry Elise! Part of my recovery involved ditching the Garmin AND the whoop. All the negative feedback was only adding to the stress. Almost overnight after several weeks it all regulated! I hope you can find some stillness and let your nervous system calm down too
Super article Whitney and awesome comments. My illness symptoms were mild – elevated temp of 99 to 100 for three days with a sore throat, some sniffles but almost no cough. Pulse Ox normal at 98 to 99%. That was followed by a week and a half of fatigue with a few sniffles and this feeling like my legs were cement – like I had never been a runner in my life. I am now three weeks out from when the illness symptoms subsided.
In the last week, I decided to test things by power walking a couple miles a couple days in a row. Had a little tightness and very minor breathless feeling on finishing that went away completely in a minute or two SO was happy about that.
I followed that up the next day with a slow 1.15 mile jog (11.5 minute mile pace) just to test things. I could tell my heart rate was way higher than normal when running and on completion (>130 a minute a minute after completion). Took me an hour to get down to my normal heart rate (42 to 46 resting). Also had palpitations immediately after for a couple minutes.
My basic physical, EKG, blood work were fine per my doc. My resting heart rate is normal though (and 02 normal) – it’s the running that raises my heart rate rapidly and way over what it normally was. Getting a cardiologist assessment in a couple weeks. I actually feel pretty good except for the elevated heart rate during/after physical activities and perhaps having a small bit of fatigue after physical exertion.
Of course, as a runner, we are wondering when the heck will heart rate adjust down to normal or will it ever? What happens to those strenuous trail runs with all the steep ups and downs or that leisurely long Sunday run? I guess only time will tell. Gotta think positive thoughts. Had to contribute to these comments and share for others in our (running) shoes since this article and the comments helped me!
Thanks for reading & sharing your experience! I hope it all calms down soon. But yes positive thoughts & just knowing what was going on & that it was common, especially in runners, helped me heal. Best of luck to you!!
This was a super helpful article, thank you! Just got COVID for the first time a week ago and was lucky to have a super mild case. However, I’ve been dealing with the increased HR somewhat at rest and definitely with running and it’s been so frustrating! I even feel great when I run except for my heart rate. Running a marathon in 8.5 weeks in an attempt to BQ so I’m hoping this clears up – if not, might have to just eat the registration fee and look forward to next year. Thanks for the write up – glad to know I’m not alone in this!
Oh man! I hope you rebound quickly!!! It’s so hard to lose that training. Is there a backup marathon later in the fall you could do? I know it’s outside the BQ window for next year but still could be a bQ!
Great article and should help getting people back to running. I got COVID first time in the first week of Jan, symptoms lasted for 15 days. Doctor recommended 3 days of rest for each day of Covid, got a heart echo and lung x-ray done, everything was normal, started running after a month and barely made it to a mile, I skipped the 3m half and the Austin marathon, I was back to my usual pace by the end of March. Completed the Chicago Marathon and on returning back got COVID again!! Symptoms were milder and lasted a week. This time I started running in a week, after a month my pace is still off by about 90 sec l, am guessing it will take another month to get back to normal. The only good thing that came out of Covid was I quit smoking and healthier diet!!
This was SO helpful and right on point with what has happened with me and COVID. I ran my best marathon yet last year in Indy (2:55:52) and had a goal to shoot for 2:50 this fall, then 3 weeks ago my wife and I both got COVID for the first time and we got it BAD. Two and a half days of fever, body aches, chills, fatigue, nasty headaches, and then a sore throat and productive chest congestion. With my first marathon on 9/11, I wanted to get back to training quickly, but when I went out for my first “easy” run a week after COVID, my heart rate had jumped about 10-15 BMP from just two weeks earlier! I’m very fit and haven’t been that sick in probably 20 years. I could tell my breathing was a bit more labored, but not all that bad. I could hardly believe the heart rate numbers for the effort I was putting forth. Also, being this is my second year working with a coach on heart rate based training, I’m very in-tune with where I need to be and my trusty Garmin and chest monitor are fairly accurate.
My coach said to rest for 3-4 days and then has had me walking more and putting in some “easy” shorter runs that are still feeling way too hard. I was hoping to have recovered more by now as I was so happy to get into the London Marathon this year via the WANDA Age Group Championships; now I am just hoping I can cover the distance so I can get my 5th Star.
As someone who eats healthy and runs year round, this has been a huge disappointment for this marathon cycle. I’m glad to not be alone in having these issues and am hopeful that my heart rate continues to improve in the next couple weeks (so I at least can get some long runs in).
I wasn’t planning on doing Boston again next year, but now, it seems that may be my next best opportunity to get back to my goal of 2:50.
Thank you for compiling this information and data!
You are not alone, Nick! Many have found that resting more early on (what they call radical rest) can shorten symptoms. Also, the HR does regulate in time even when running! For me, an inhaler & steroids helped!
So very helpful. IronMAN here (M48). RHR was 53, post mild Covid 3 weeks ago (fever, some drainage for 48 hours), RHR 79+. Running zones have moved by AT LEASE 1 zone in the wrong direction now. Zone 1 is now Zone 2, Z2 is now Z3, etc. Labored breathing (heavy chest) all the time even though I have .5 liters larger lung capacity than the avg male.
Very few search results are covering this from a runners POV. Thanks for the info from you and everyone here.
I hope you recover soon! In most people I know (myself included), it resolves in time! An inhaler in the meantime can help with the breathing.
You can add me to the list of people who are feeling very grateful to have found this article! I’m a run-walker (10 min run, 1 min walk) who has done quite a few half-marathons and have been contemplating my first marathon. I’m not new to heart rate issues – my RHR was often in the low 40s, but it would go up a lot during my runs (one of the reasons I walk). A cardiologist did a number of tests on me last year and found nothing abnormal about my heart, so it was just something I lived with. I got Covid at the beginning of June, despite being triple-vaxxed, etc. My symptoms weren’t too bad, and I got back into the swing of things after a week or so. But I noticed that my RHR had gone up by about 20BPM, and my exercise heart rate was also up even higher than usual (when it’s already pretty high). I was managing it – running slower, making my run intervals even shorter, etc – but then I got another cold/flu bug (not covid) that lasted a couple of weeks, and that seemed to set me back again. The last couple of days, I’ve run super slowly, taken a lot more walking breaks, walked on the hills, etc. but my average heart rate is still super high. I think I will go to the doctor to look into it, but this article does give me some assurance that this is not unusual for runners who have had covid. I already have inhalers due to asthma, but I may also look into deep breathing exercises to see if that can help. I hope that I can get back into the swing of things soon, b/c I have been quite discouraged by how much I’ve struggled during my runs, and I’ve been nervous about increasing my distance beyond 10k.
Hi Alison,
I am sorry to hear you are having trouble too. I think going to a doctor to get checked out is definitely a good call and can maybe give you some reassurance and potential management strategies. As I mentioned, time and then knowing everything will eventually regulate helped me a lot because I was freaking out at first! I hope you can run without worry soon! Whitney
Yea thanks you all, made me a little more calm now.
Same experience as most people here.
Fairly good runner from 10k up to marathon, M45, had minor Covid, and after that 10-15 beats elevated HR for weeks now.
Also poor sleep?!.
Have been training, But taking it easy.
Has anyone gotten back to normal RHR and how long did it take?
Ah, I am sorry! Yes, most I know have but timescales vary. It took me about 6 weeks.
Ok, Nice to have some kind of timeframe. The one thing I am still wondering about, is it any danger of training, and sometimes train somewhat hard, at least as long as it feels comfortable and no other issues. That I have not read anything about.
Take care you all!
That is a question best answered by your doc of course–but from what I have been told, if it is only an elevated HR (no other issues) you are okay to continue to train!
Cheers Whitney, ill keep an eye on it!
Question – how elevated of a HR during exercise is okay and normal (if no other symptoms)? I’m probably at least 15-20 bpm above normal during running at this point.
Hi Whitney,
Really appreciate you writing this article.
I’m on week 5 from my initial Covid symptoms and still have an elevated heart rate both resting and while running (or more like jogging right now lol) I’m praying that i follow in your footsteps and the old ticker goes back to normal after 6 weeks!
Hi Chad, I am so sorry to hear that. But I am hopeful all will resolve. I’ve had several athletes with similar issues and all regulated in time!
Great article (and so sad so many have been affected) and very informative. I am a 72 year old triathlete (30+ years and counting). Had an afib event, my cardiologist checked me out (stress test, echo, 7 day monitor) and said all was fine. Then I got covid (pretty bad code like symptoms) and resting HR, HR variability and max HR all have been affected (and I have tons of historical data from my Garmin 935). So almost 4 weeks from testing positive (and 2 from testing negative) I’m back to mild exercise but resting HR is 20 over past norm, swim and bike are higher as well but the few runs I have done at a much slower pace get my HR to max within a minute or two. Am seeing my cardiologist again end of November and am hoping being smart and handling this as a ‘watch, monitor, wait’ issue it will resolve itself. Thanks again for the very valuable information that has been posted.
Thank you for this. I am a very fit 61-year old female. I’ve been getting into running; started with MAF and was doing fabulously and adding in longer runs and hill interval training (getting up to 5 mi runs and ave pace of sub 9:00 min/miles keeping my HR in a good zone). Got COVID mid October while in Portugal. Fairly mild case (did have low grade fever for 2 days) and was able to keep active (walking) throughout COVID. Came home and started back with MAF and had to walk 75% of it. Took a week off and concentrated on brisk walking, using MAF-10. Today was the first day I tried to do a “long” or consistent run. 1-mile @ 11min/mi. Ave HR was 131 with a high of 152. This is more like my pre-COVID 9min/mile HR. While I was running, it felt okay and my HR recovered okay. Not sure if I should go back to walking? walk/run/walk/run using MAF formula or run 12-15 min 3x/week at a slow rate that feels okay and not worry about HR. I have put a note in to my PCP — otherwise I feel okay . Would love some suggestions about how to proceed!
Thank you for this! It’s so reassuring to hear from other athletes about their experiences. Family doctors just don’t have the knowledge on how to guide people back into this type of exercise I find, so it can be scary. Having to convince a medical professional that a high 50s resting heart rate is extremely abnormal for my body is hard! I’m one of the people that still has chest pain and extremely high heart rate several weeks after covid, but with all tests coming back fine my doctor had no real advice on if I am okay to ramp up to my normal mileage or not.
I have had the same experience. The only thing is that I never tested positive for COVID. I ran the Berlin Marathon at the end of September and then was supposed to run NYC ( I ended up deferring). I felt crappy two weeks before Berlin, but I never tested positive and I felt better within two days of running Berlin. Halfway through the race, my heart rate spiked and was between 185-200 bpm for the last two hours (I had been running my usual long run pace to start @160 bpm but slowed down significantly when my heart rate spiked and finished). Afterwards, I took some time off and then started trying to train for NYC and I never felt “normal” again. I thought it was overdoing it from the marathon, but my heart rate was consistently higher than usual even when I was running over a minute slower than my usual super easy pace. Now it’s been 8 weeks, and I have taken a lot of time off but I keep trying to run 3-5 miles and it’s too much. I tried to run a 5k last weekend (7 weeks after Berlin and most likely my recovery from COVID?) and I was so slow and my heart rate was 194bpm avg. I’m going to try to dial it back and see if I can get back to normal by following your suggestion of just walking and doing a mile or two very slow with lots of recovery in between. I have been to the doctor multiple times and they have no idea what’s going on and now I have an appointment with a cardiologist, so hopefully I can get a hold of what is happening between seeing the cardiologist and just taking it slow.
Thanks for this article and the research you did. One month after what was a pretty mild bout of Covid my heart rate while running is still 15-20 BPM higher than before. No pain or difficulty while running (except for obviously having lost conditioning) but I’m 74 and was concerned. This puts me somewhat more at ease, but I will continue to monitor and consult with my dr. if I experience anything else or it doesn’t begin trending down. I’m wondering though, does this suggest that when I do recover more I can consider running at a higher BPM than I used to?
70 year old 8,000 mile a year cyclist who also walks/hikes 500 miles annually. Resting HR normally low 40s, 38 in middle of night. Post-COVID HR steady mid-60s, and Z2 effort now 30 bpm above normal.
Z3 efforts and higher seem to set recovery back. New Years resolution is to take the recovery more slowly.
Reassuring but also disturbing to see so many others dealing with same symptoms.
Best wishes to all, and thanks much for this outstanding article.